The majority of people with CMT have the 1A subtype which is due to duplication of the peripheral myelin protein 22 (PMP22) gene leading to breakdown of the myelin that surrounds peripheral nerves. With time this loss of myelin causes nerve dysfunction and degeneration resulting in loss of sensation, weakness and loss of muscle mass.
Today scientists are testing a number of different therapies for CMT 1A that are at various stages of development. The ultimate goal is to develop disease-modifying therapies that slow down, stop or even reverse the course of the disease.
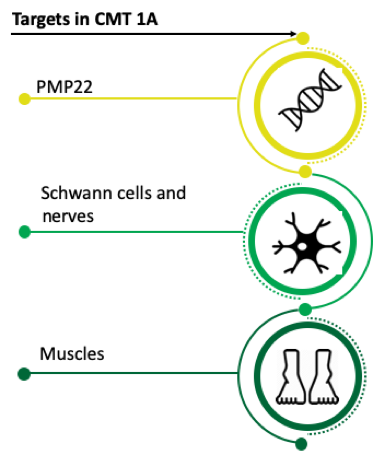
Targeting PMP22
Multiple methods are being tested in animal models and in humans to determine whether decreasing PMP22 in the peripheral nervous system is effective in treating CMT 1A. Therapies that target PMP22 directly must be carefully modulated as not having enough PMP22 in peripheral nerves also causes neuropathy.
Using Small Molecules to Modulate PMP22
Small molecule therapies typically are developed from simple building blocks or are derived from natural sources. With their small size, they are easily able to pass through the cell membrane and access targets inside the cell.
- PXT3003 is in late phase clinical testing by Pharnext and is an orally administered combination of three different chemicals- naltrexone, baclofen, sorbitol- that each act through a different mechanism to lower the levels of PMP22.
- Addex is developing and testing a GABAB receptor activator in rodents as a way to lower levels of PMP22.
Gene therapy to lower PMP22 in the peripheral nervous system:
Gene therapy treats disease by modifying the genetic machinery of cells in the body thereby targeting the underlying genetic cause of disease.
- Ionis has tested an anti-sense oligonucleotide in rodents that successfully lowered PMP22 and had beneficial effects on nerve function.
- The CMT Research Foundation is funding Kleopas Kleopa, a leader in the field of gene therapy for CMT, to develop a viral-mediated gene therapy approach which has the potential to be a long-acting treatment.
- Permanently modifying the regulatory elements in the DNA that control expression of PMP22 via gene editing using CRISPR/Cas9 was recently tested in a rodent model of the disease and led to preservation of myelin and axons if treatment was performed before signs of the disease.
Targeting Effected Nerve and Muscle Cells
Other potential therapies target downstream cellular processes that lead to nerve dysfunction, degeneration and muscle weaknesses. These include targets in Schwann cells, peripheral nerves and muscle.
- The small molecule, MD1003, a form of the B vitamin biotin, targets the enzymes involved in energy production and the synthesis of fatty acids essential for myelin in peripheral nerves. MD1003 would be expected to increase myelin production and help nerves function better.
- IFB-088 (also called Sephin1) is an orally active drug that modulates a normal stress response in cells called the unfolded protein response (UPR) which is triggered by abnormal proteins. IFB-088 helps cells to better process abnormal proteins and may help preserve nerve function.
- MP-188 acts to block a protein contributing to elevated levels of intercellular calcium thereby reverting the function of peripheral nerves back to that seen in normal cells.
- Neurotrophin 3 (NFT3) is a growth factor that improves nerve regeneration and myelination and is delivered via gene therapy and is currently in early stage clinical testing.
- CLZ-2002 is a type of cell therapy wherein Schwann cell-like cells are injected locally near specific nerves to help with remyelination of the nerve.
- ACE-083 is in late stage clinical testing and is injected locally into specific muscles and inhibits select proteins that reduce muscle growth. Inhibiting these proteins is believed to increase muscle mass and strength in the muscle where the drug is administered.
The speed of therapy development is increasing and we are hopeful that the first therapy for CMT will be approved in the near future.
by Grace Pavlath, PhD, Chief Science Officer for the CMT Research Foundation
